During our final critique last night, many of the comments of our proposed app addressed concerns about the reliability of patients’ self-tracking information. In other words, will a patient honestly report that they have taken their medications and followed their exercise and diet plan for that day? Most comments acknowledged that we could link our app to different programs such as a Fitbit, a Nike fuel band, and prescription refills to monitor whether a patient was actually fulfilling their treatment plan. These modifications would provide objective data that the patient is following through with their treatment plan.
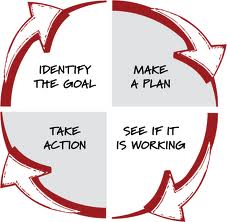
While these modifications would definitely streamline the process of providing correct information, I think they miss one of the most valuable aspects of self-tracking. Since I our app, the patient has to check off which aspects of their treatment plan they followed during the day, it automatically forces them to reflect on their day and their progress in achieving their goals. If the information automatically syncs to the app, it eliminates a crucial step in the goal setting process, which is reflecting on your current progress in achieving your goals.
The problem can be viewed from two different perspectives: the patient perspective and the physician perspective. From a physician’s perspective, it is extremely useful that the automatically recorded data would provide objective findings on a patient’s progress. A physician could see that a patient is only running once every two weeks from the information provided in a fit bit or other device. It reduces the need for the physician to rely on accurate self-reporting by their patients. From a patient’s perspective automatically reported data reduces time spent self-tracking, but it ultimately doesn’t make the patient more engaged in their treatment plan and illness.
If we move towards an app that relies less and less on patient self-tracking it also moves away from a collaborative physician-patient relationship. The goal of our app is to create a shared-decision making tool that can be used at the clinical encounter. We wanted to move away from the historical physician-patient relationship which is very unidirectional. In this model, the physician tells the patient their treatment plan, and the patient follows that treatment plan. The purpose of self-tracking is to have the patient track their health to make them more engaged and better able to manage their condition. If we remove the physical process of entering in information, we risk losing patient’s engagement and thus decrease a patient’s responsibility of their own health.