Recommended by: http://it-is-a-3-patch-problem.tumblr.com/post/57732674295/thought-this-may-be-useful-for-a-few-people-on
Category Archives: Technology
Sleep Profiling
http://www.bbc.co.uk/science/humanbody/sleep/profiler/
The National Institute of Health estimates 50 to 70 million American’s sleep patterns suffer from sleep disorders and/or intermittent sleep problems. That means that nearly 20% of Americans are having trouble sleeping! Whether from their environment, their psychological state, or their health issues, a significant portion of America is going to class or work foggy from fatigue.
At the above link, via the BBC, you can take a sleep profiling quiz (regardless of whether or not you believe you’re a part of that 20%) that will determine how well you’re sleeping and what adjustments you might want to make.
Personally, I was recommended to remove my computer and stereo from my bedroom in order to remove temptation from activities that will stimulate my brain too much right before bed.
This has been recommended to me before by friends, but seeing the data before my eyes of my sleep schedule compared to how often I doze during the day allows me to solidify in my brain what is wrong with my sleep schedule.
This sort of online survey can quickly and easily create an e-patient in terms of such sleep issues, and is something I would particularly recommend to busy students!
Quantify Yourself
As Socrates once said, “to be is to do.”
As an aspiring physician, I’ll soon enter a clinical environment that’s more data-driven and technology-oriented than ever before. More patients are using mobile applications to track their health data. More providers are incorporating patient-generated big data into clinical decision-making. More devices are becoming integrated into the Internet of Things, a connected contextual framework with the power to drive personalized, predictive healthcare.
In class, we’ve discussed how e-patients can use self-tracking to build awareness and control over their health status. In our design setting, we’ve examined how intensive care physicians have to consolidate vast quantities of data into a cohesive patient narrative and a plan of care. But there’s discussing and observing, and then there’s doing. I decided to take it a step further. I wanted to situate myself in the patient’s, or provider’s perspective, using self-tracking to inform and inspire my own health behaviors.
Over the past 30 days, I’ve used Azumio’s Argus to construct a digital timeline of my lived experiences. Every morning, I log my sleep, heart rate, and blood pressure. As I walk across campus, I measure my steps and calorie consumption. When I sit down for a meal, I take a snapshot of my plate. With each meal, I record how many glasses of soda and/or water I’ve had. When I hit the Rec Center, I record my exercise by type and duration. If it’s a weeknight study session, I count how many cups of coffee or tea it takes to power through it. If it’s a weekend, as I hit the bars, I save how many bottles of beer or glasses of wine I’ve had. And at night, I check my pulse and blood pressure again right before my head hits the pillow.
Now, the critical question: what have I learned?
Commitment. Between Week 1 and Week 4, my “compliance” fell from 96% to 63%. It takes a committed, conscious effort to record every meal, every vital sign, every exercise, every minute of the day. I hold a new-found respect for the diabetic patient who has to monitor his blood sugar, manage his appointments, and mind his meals; it’s a process that’s both distracting and exhausting.
Awareness. As much as the constant inputs were a challenge, they empowered me to become cognizant of my daily behaviors. Did I really eat pizza and chips for lunch that often? I went that long without drinking water? Do I really spend so much of my day in a sedentary state? To record empowers us to know, and to know inspires us to act. I wonder if, as we move towards ‘ambient-tracking’ devices, we’ll lose this sense of awareness and agency.
Application. So often I found myself asking, what really matters? Argus would frequently warn me that I hadn’t drank water in three hours, or congratulate me for walking 10,000 steps that day. Did these things necessarily make me a healthier person? As we realize our ability to quantify everything, it’s important for us to isolate signals amidst noise. It’s necessary that we identify the parameters that matter for health versus those that don’t. It’s vital that we appropriately calibrate the thresholds of behavior that justify a congratulatory or cautionary alert. Data for data’s sake is useless; the next step is to make that data actionable.
If you haven’t quantified yourself yet, it’s a must. Data is a ubiquitous element of our modern lives. When we quantify ourselves, we can critically evaluate our daily experiences from a birds-eye vantage point. We can channel those insights into knowledge and action to enrich our lives. And, as future physicians, we can learn what it means to gather data, make sense of data, and use data to drive clinical decisions.
Ping. Have It Your Way.
Ping. That must be my daily reminder. How am I feeling now in terms of arousal and valence? Well, I just had my weekly meeting with my research advisor. He was really getting into the nitty-gritty and suggested that I should have been farther along with my project. I don’t even like this project. I wish I could just get it over with… Anyway, probably low valence. It was a pretty negative experience. Also high arousal… He really stresses me out, and I could feel my blood pressure rising.
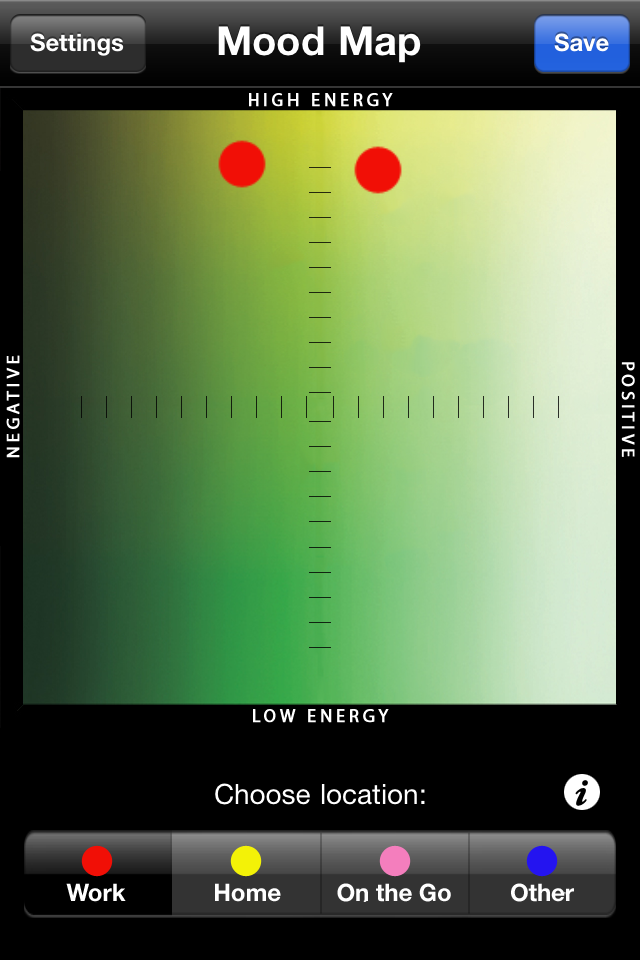
Photo Credit: mzstatic.com
One of the greatest benefits of mood tracking is increased self-awareness. Mood tracking apps like Moodscope and Mobile Therapy remind users to take a step back and to reevaluate their life choices. They can reflect on what is bringing them happiness and what is bringing them down. By connecting their moods with other factors happening in their lives, users can develop a greater understanding of themselves with respect to their environment.
The beauty of mood trackers is that they also provide spatial and temporal information. Users can link their moods to their immediate spatial surroundings and to the time of recording. By randomly sending pings throughout the week, these apps can help users determine where and when they tend to feel upset or happy.
Additionally, mood trackers do not only take in information, they can also offer advice. Mobile Therapy offers therapeutic exercises, including breathing visualization and muscle relaxation. It also offers strategies to quit smoking, treat anxiety, and detect relapses in psychotic disorders. Ideally, these mood tracking apps could personalize therapeutic exercises to a user’s specific input. You could “have it your way” by inputting end goals, such as cultivating happiness or controlling the relaxation response.
Photo Credit: play.google.com
With most mood trackers, it is also possible to add information through texting—users can share paragraphs of information if they feel inclined to do so. Therapists and physicians could use these self-reflections to see how their patients are doing over time. Appointments with health professionals are short, and they are not necessarily indicative of how the patient normally acts. Some patients may experience white coat syndrome, so there is an additional benefit of having records of patients outside of the doctor’s office.
In the future, perhaps these apps could notify the patient’s physician directly. Jon Cousins describes the benefits of connecting his data to those close to him: “We leave traces of ourselves with our numbers, like insects putting down a trail of pheromones, and in times of crisis, these signals can lead us to others who share our concerns and care enough to help.”
If physicians have access to their patients’ personal information, they can individualize their treatments. While there would be a lot of information to handle, this issue could be alleviated with efficient organization and clean programming. It is possible to automatically assemble the relevant information in a visually aesthetic way, and these apps track not only the physical health of users, but also their mental and psychosocial health.
Looking Into ePatient Outlets: PatientsLikeMe
As a continuation of my first blog post discussing CrowdMed as a possible ePatient outlet, defining the movement with a community of curious patients and a medically educated crowd base, this time I will focus on PatientsLikeMe to provide a different approach.

PatientsLikeMe is a free public website that provides a patient, clinician, or caretaker to register and provide, receive, and share health information. Users are able to input symptoms, medications, and treatments to find people undergoing similar medical situations. Communication is facilitated through both a forum type infrastructure and user comments.
Individuals are able to search the information database for not only patients with similar symptoms, but also for a wide range of medications and treatment opportunities for a particular condition. Treatments can be searched based on frequency of use amongst patients, user rating, efficiency, and side effects. In addition to medical and pharmacological solutions, users can browse through dietary, physical activity, or mindfulness treatments suitable for their personal needs.
In addition to acquiring a wide range of helpful information, the website allows people to track their health and invite others (doctors, family, friends, etc.) to their “care team” and share the status of their health. The tracking information can be easily be shared with those not on the website through an easy print format which the individual can choose to print or email to someone else.
The website automatically stores the shared health history to a database to match the user up with pertinent clinical trials or be used for research.
Different from CrowdMed, this ePatient outlet is geared towards personalizing one’s involvement in sharing and receiving health information. The website is structured so that all information provided by other users is easy to understand even with low health literacy.
PatientsLikeMe is very attractive in that everything from health tracking to research can all be done under one website. With the ease of having access to variety of resources in one spot, the site is able to lower some effort barriers that may restrain patients from transitioning into ePatients.
This ePatient outlet definitely highlights the empowered definition of the entire ePatient movement, giving the individual full control over their involvement in how their personal health information gets used and how they themselves act to provide for others within the virtual community. Involved users are not only free to educate themselves with healthcare options that can easily be discussed with a physician, they are, in addition, given the chance to take their health into their own hands with clinical trials and nonmedical treatments such as wellness exercises and stress management.
If CrowdMed is a helpful resource for finding answers under the ideology of “power in number”, PatientsLikeMe is the example of self-driven medicine with an interface chosen by the user’s preferences. This is a great illustration of patient empowerment, as patient empowerment is not only choosing what to be involved in, but choosing the threshold of involvement as well.

