Google recently announced a project in which they plan to develop contact lenses that measure a person’s blood glucose level. The project is very much in the early stages of development but it indicates the potential for furthering involvement of technology in healthcare. It is imperative that the healthcare industry supports technological innovations such as this that will improve patient care. Technology must be viewed in the same way as medication in how beneficial it can be to global health.
Google describes the project as a potential game changer for diabetes treatment. The function of the contact lens is to measure glucose levels in tears, thereby making it easier for diabetes patients to determine their blood glucose level. At the moment, a patient must draw his or her blood which can be a difficult and painful process. What ends up happening is that patients fail to regularly check their blood as often as they should and develop further complications as a result. How the data from the lens is made known to the patient is not currently established. Some have suggested a series of blinking lights in the lens that notify the wearer when it is time to take insulin. Another approach is to somehow transmit the data to the user’s smartphone where it is displayed in an application and stored on a secure Google server. In the latter solution it would also be possible to send this stored information to the patient’s physician, providing them with updates on the patient’s progress and insulin usage. A cutting-edge solution to treat diabetes more effectively is vital considering it is one of the fastest growing diseases in the world.
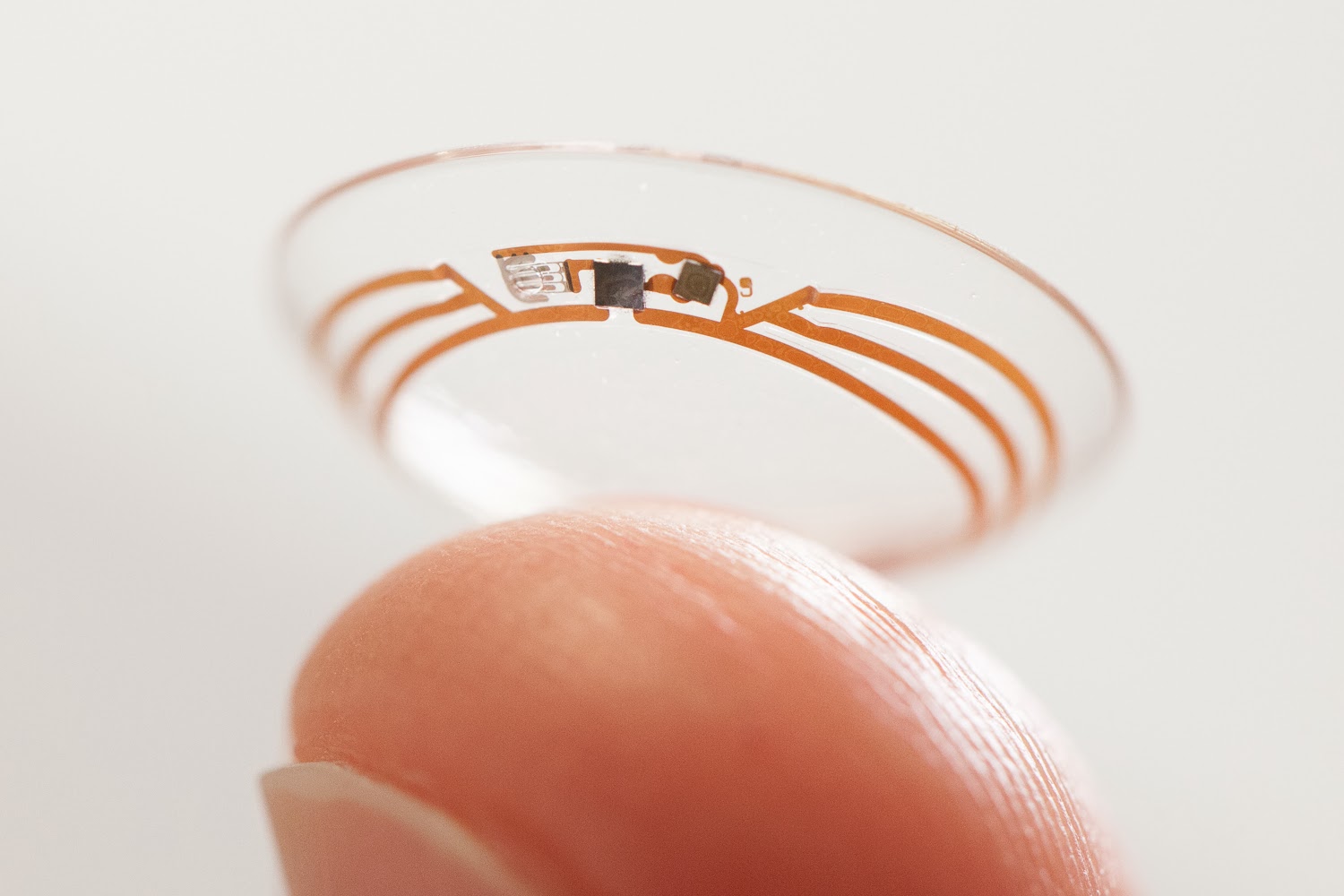
In this modern age of technology and rapid development of new and exciting products that better quality of life the healthcare industry must be more open and supportive of innovation in patient care. Not to say that it is currently averse to the prospect but there exists a lot of red tape and inefficiencies that slow progress. The industry must be willing to adapt as quickly as the rest of the economy in order to realize vital improvements that will help patients today. The laggard mentality and outdated ideals prevalent in the healthcare system must adapt to the current culture of innovation and ubiquitous use of high-tech devices. This will ensure projects such as the Google contact lenses become tangible products.