Cancer and cancer treatment leaves a trail of digital data. I’ve been thinking about this digital trail today, and the different forms it took for me during my diagnosis and chemotherapy.
MyMDAnderson
This is my personal MD Anderson portal. Though I never bothered to check on my documents very often, they are are available online, like pictures in a scrapbook. Looking back on them now, I’m intrigued by sheer the volume of the data MD Anderson collects on me. There are patient reports for every meeting and consultation, notes on every interaction.
During my first echocardiogram, the technician applied gel on my chest and asked an innocent question: “so, you’re an Ecology and Evolutionary Biology major?” I was instantly taken aback. I had never seen the man in my life or mentioned my major. But everything I told my oncologist had been stored for future reference, even the information I considered mundane. I often think about this interaction when we talk about how doctor-patient interactions should improve. The question about my major was unsettling to me rather than indicative of warmth and caring. It implied a greater, almost sinister, system of knowledge that I had not considered before then. Though the question was intended to be intimate, it “revealed the trick” and made the interaction seem alien and forced.
Texts
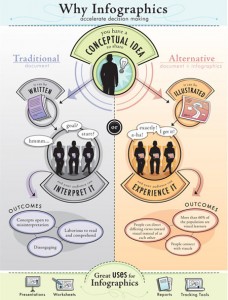
I sent many messages, both in text and photograph form, in the earlier stages of diagnosis. They weren’t really to alert my friends and family to my progress, and they weren’t really to stave off anticipation and fear with regards to treatment, at least not consciously. I just had an obsessive desire to share the new events and experiences that were occasionally humorous, as in the case of the apple-flavored barium swallow, or the nurse who assured me that the radioactive glucose used during PET scans was “just a bit of sugar water, like they give to hummingbirds.” It turned out that image texts were the most immediate and easy way for me to convey information, and what I usually used. The trail of texts did die off towards the end of my treatment, however. I was tired. I felt I had less to say. This is in line with what I’ve heard from many current and former patients: when you’re feeling sick, you don’t want to interact with technology and others.
Google Searches
This one is less obvious, but still there and very important. I was constantly researching my diagnosis, symptoms, side effects of chemo and biotherapy. These will influence my future search results in ways I may not necessarily anticipate now.
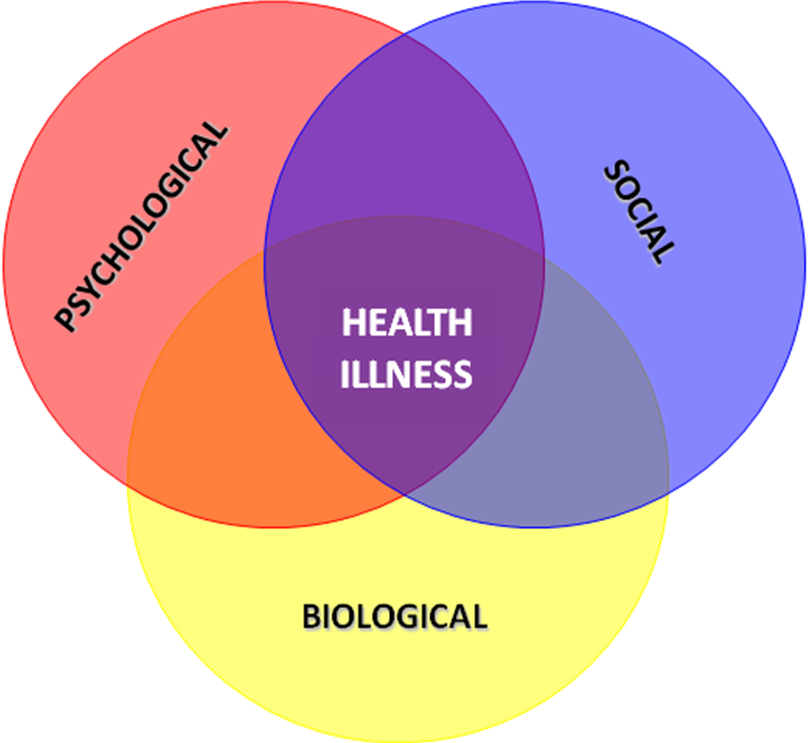
Many communication problems in medicine require tailoring the solution to the individual patients. Some may want warm and caring doctors, others want their physicians clinical and direct. Some may engage eagerly with apps, while others have trouble mustering the motivation to get out of bed. These sorts of digital trails provide several unique perspectives: the medical and physiological angle, the relationship angle, the personal and introspective angle. How can we harness and combine these perspectives to create better solutions? And how can we respect privacy and patient concerns while we do so?