One of the topics that we have discussed on varying occasions throughout the semester is electronic health records (EHR) and how they interact with and effect patient care. In my own groups work with our problem owner in the CV ICU, interaction with the EHR has been a large part of developing a solution. As I have continued to work with and research the present systems, I have noticed, both in the classroom and in the hospital environment, an inconsistency in terminology used to refer to the records. From what I observed, the terms electronic medical record (EMR) and electronic health record (EHR) are often used interchangeably. Curious, I looked to see if there was an actual difference between these two records and how they are involved in medicine.
Google Trend Data Tabulating Searches for “EMR”and “EHR”
Though these terms are often used synonymously, there are marked differences between EHRs and EMRs and how they are used within the medical field. My research led me to discern that the term EMR refers to essentially a digital version of the paper charts that they replaced. These digitalized systems contain a patients medial and treatment history specific to a doctors practice and posses the ability to allow caretakers to track data over time, identify which patients are due for screenings or appointments, and monitor quality of care within the practice. The largest difficulty when using EMR is transfer of information out of a physicians practice, and in that sense does not improve significantly from a paper record.
So how do EHRs differ from what I have just described? The key difference between an EMR and EHR is the focus of use. As described by a variety of sources, an EHRs functional aim is to address the total health of the patient, going beyond the original health organization to encompass information from other health providers including laboratories, specialists, and most importantly the patients themselves. The ability to share information in a secureway throughout all aspects of patient care creates the possibility for interactive communication and the meaningful use of EHRs as a tool to improve patient care.
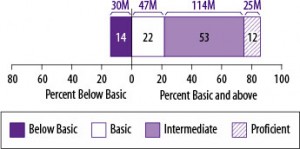
Overall, what I found is that while the terms EMR and EHR only differ by one word, that small change makes a world of difference. The engagement and commination opportunities that the EHR provides, makes a case for the use of these systems exclusively. A push for providers to engage patients through their access to the EHR system has occurred in recent years, but is this engagement really effectual and beneficial to patient care? With an estimated 77 million Americans that possess either basic or below basic health literacy, are EHR systems providing accessible and useable information to patients to improve their care or are many patients just getting lost in the process?
To answer that question the Agency for Healthcare Research and Quality have examined health education materials delivered by EHRs and have determined that many do not often account for the poor health literacy possessed by a large amount of the population. So what can we do to make EHR systems more useable for patients and improve care outcomes?
A number of leaders of Health IT have begun address this disparity by suggesting a list of preliminary standards and key tools designed to be incorporated into the existing and new EHR systems. A number of simple changes to improve direct communication with patients include providing patients with the ability to identify their preferred language. Other functions including the ability of EHRs to filter quality measures by patient characteristics such as language, socioeconomic status, and education level, could work to reveal and address disparities in care, including those involving health literacy. In addition to providing better resources for patients, having EHRs include information such as disability status, sexual orientation, or gender identity can provide caregiver a greater context regarding a patient’s health recommendations and outcomes. While these changes serve as the initial push in addressing functional and health literacy changes to EHRs, there are still ways to improve the educational value of the interactive system.
What other innovations could be incorporated into EHR systems in improve health literacy?