Self-tracking devices have been lauded as the potential solution to filling in the gaps in traditional clinical data collection. Oftentimes, measurements in the doctor’s office are not truly indicative of the patient’s everyday behavior and lifestyle; patients may experience white coat syndrome, or increased anxiety in the presence of the doctor. Automatic self-tracking in everyday living may provide more accurate data because the data is collected in more natural settings.
One of the goals of self-tracking is to model and predict human behavior. This sounds quite promising; however, how does this automated self-tracking actually come about? Would we want our personal handheld devices to predict our next moves? And what a fascinating thought experiment it would be to have our phones, these inanimate devices, give us life suggestions. But oh wait, they do.
Google Now carefully watches its users’ every interaction to improve its efficacy. It can predict where you will go judging by your past behavior. It can detect that on Wednesdays, you like to get a Grande green tea frappe at Starbucks before your Russian literature class, and sometimes, when you’re having a particularly packed week, you treat yourself and venture into the bold Venti end of the spectrum. While Google Now has the potential to notify you if there is a promotion on green tea frappes, it may suggest another drink perhaps, and as a subtle suggestion, a drink with fewer calories and a lower fat content.

Photo Credit: clipandfollow.com
Popular Science awarded Google Now as the 2012 “Innovation of the Year” for its potential to serve as an “intelligent personal assistant.” It can infer your age bracket from your recent searches and tailor advertisements to your curated predilections. For your mother, it can suggest her favorite hair dyes or jewelry boutiques, but what if one day following her sixtieth birthday, it begins suggesting cholesterol medicine and life insurance? While this teeters on the edge of being mildly insensitive, it may regrettably be a sensible recommendation.
But it doesn’t stop there. Google Now has a minute-by-minute map of your life. Not only can it suggest nearby attractions and events, but it can also summarize your daily physical activity. Given your latest late-night food adventures, it could now suggest restaurants with healthier vegetarian options. It could also suggest a route that requires more physical exertion (to make up for that discreet donut run that you thought went undetected), and in your hurry, you wouldn’t notice that it was slightly more strenuous, with a steeper incline of about two degrees.
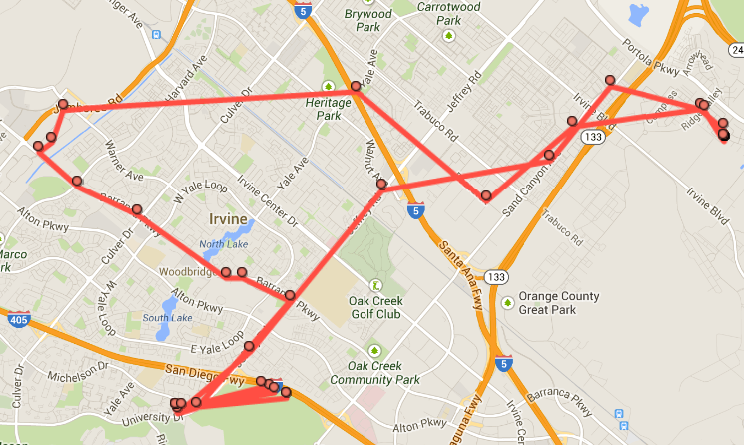
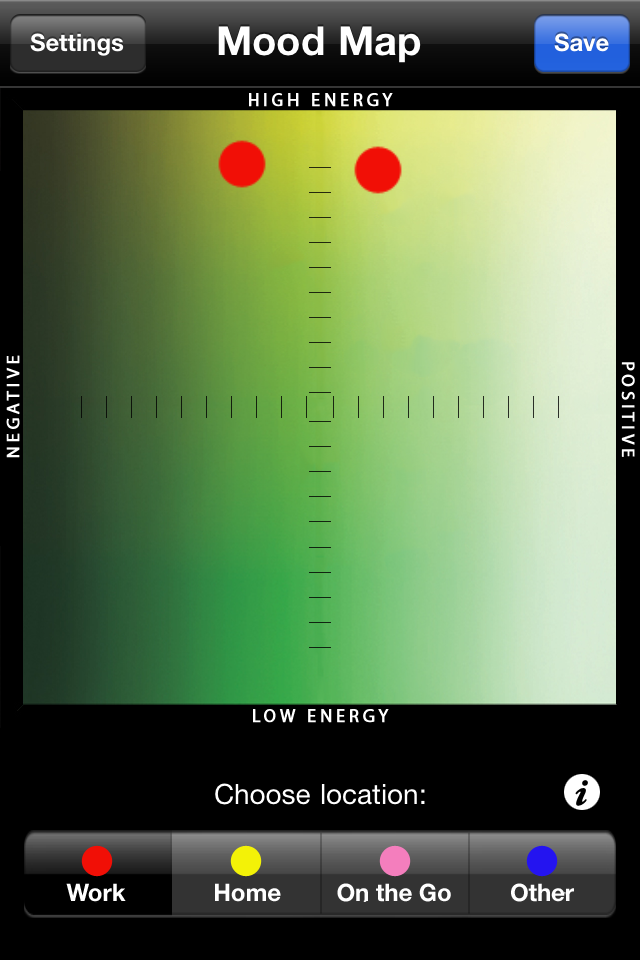
Photo Credit: geofffox.com
Physicians have the potential to produce mobile health applications that use the same tracking devices as Google Now. While they have the promise of displaying customized content and advertisements, they can also subtly suggest healthier eats and longer walking routes. With smartphones constantly linking accounts and contacts, mobile health applications will soon be connected to the information collected by Google Now. And suddenly, without your conscious awareness, you will be forced to be utterly and irrevocably healthy.